 *1 †
*1 †Research Articles
Educational Training and Services Provided by Hearing-aid Specialists in Spain: A comparison with the General Audiologist Model
1Vanderbilt University, Hearing and Speech Sciences Department, Nashville, TN (EE.UU)
2Midwestern University, Department of Speech and Language Pathology, Glendale, AZ, (EE.UU)
 OPEN ACCESS
OPEN ACCESS
PEER REVIEWED
ORIGINAL ARTICLE
Abstract
The vocational training certificate in Hearing-Aid Specialist (HAS) was created in Spain in 2001. During this time, university programs in audiology have emerged in the form of university-specific postgraduate degrees. However, the undergraduate program in general audiology does not exist in Spain yet. The objective of this study was to examine the workplaces, services offered and the self-perceived quality of training of HAS with and without a additional university studies and to explore whether any of these professional profiles conduct activities of the “general audiologist” role that was proposed by the European Federation of Audiological Societies (EFAS).
An online questionnaire was completed by 255 HAS. Analysis of variance was used to compare responses between HAS, HAS with an undergraduate degree in audiology-related discipline, HAS postgraduate qualifications in audiology, and HAS with both additional qualifications.
Regardless of their level of education, most HAS indicated that they work in hearing aid centers fitting hearing aids to adult patients, for which they perceived themselves as sufficiently trained. The most educated HAS indicated working in specialized centers and providing services to pediatric patients more often. Highly educated HAS also reported a better self-perceived training on cochlear implants than HAS.
In general, HAS do not receive training or offer services in areas within the competencies of the general audiologist according to the model proposed by EFAS, such as cochlear implant programming or diagnosis of vestibular disorders. Future studies focus on exploring the training received by professionals who offer this type of audiological services in Spain.
Keywords
Hearing-aid Specialist, audiology, training, education, audiological services
Clinical Implications
In Spain, the majority of hearing aid specialists work on hearing aid or optical centers specialized in fitting hearing aids to adult patients. In this type of centers, they implement good practices and feel competent developing their clinical practice. However, despite that some of them receive graduate education in audiology, they do not implement clinical practices characteristic of the general audiologist as proposed by the European Federation of Audiology Societies (EFAS). This could have clinical implications because it is unknown which professionals are currently implementing the general audiologists’ clinical practices, the quality of their training, as well as the quality of the services offered. A more detailed analysis of the audiology situation in Spain is required. Specifically, it is necessary to examine the services as well as the professional’s clinical competencies to determine whether it is necessary to formally incorporate the general audiologists to the Spanish hearing care system.
Received: 07.10.2021 Revised: 02.11.2021 Accepted: 22.11.2021 Published: 30.12.2021
Edited by:
Miriam I. Marrufo-Pérez
Universidad de Salamanca, España
Reviewed by:
Francesc Roca Ribas
Hospital Universitari Germans Trias i Pujol, Spain
Daphne Marfull
University of Valparaiso, Chile
Jose Luis Blanco
Demant Ibérica SA, Spain
Introduction
The increase in the prevalence of hearing loss in society has increased the number of professionals and training programs in the field of audiology (Goulios, 2010; Goulios & Patuzzi, 2008). As a result, after identifying a precarious situation in hearing health services, the European Federation of Audiological Societies (EFAS) published in 2001, the General Audiologist model (GA), which was recommended to be implemented throughout Europe (EFAS, 2001). This initiative aimed to create a new professional figure that had the competence to offering audiological services that until then were provided by a diverse group of health professionals (e.g., otorhinolaryngologists or ear-nose-throat doctors [ENTs], medical audiologists1 or hearing-aid specialists). These competencies included the diagnosis and treatment of hearing loss, as well as the evaluation and treatment of tinnitus or vestibular disorders (EFAS, 2001). Given the broad perspective of the GA, the competencies of ENTs, medical audiologists and hearing-aid specialists partially overlap with those of the GA. For example, while GAs and ENTs have competence to perform an otoscopy, only ENTs are trained to treat the outer and middle ear infections. It should be noted that the specific competences of each of these professionals may vary according to the current legislation in each country. Nevertheless, the audiological evaluation and treatment must be carried out by an interdisciplinary team. It is recommended that the GA serves as the interdisciplinary team coordinator, delegating medical and surgical aspects of treatment to ENTs and/or medical audiologists. The GA also oversees the hearing-aid specialist activities (American-Speech-Language-Hearing Association, 2020; EFAS, 2001). Therefore, the GA can carry out his/her professional activities in a variety of work environments, from hearing aid centers, fitting hearing aids, to private ENT clinics or hospitals focused on cochlear implantation.
In Spain, the EFAS recommendations triggered the creation of a Hearing-aid Specialist (HAS) vocational training certificate 2 in 2001, which did not exist until then (Royal Decree-Law 1685/2007). However, it was considered unnecessary to create an official university program (undergraduate or graduate degree) in general audiology. It was established that the diagnosis and treatment of hearing loss via hearing aids could be performed by HAS, while other audiological services not related to hearing aid fitting (e.g., cochlear implants) would continue being offered by professionals from audiology-related disciplines, mainly ENTs and other medical professionals (Order SCO/1262/2007).
Despite the lack of recognition of the GA, graduate degrees have emerged in Spain in recent years. These studies take the form of university-specific postgraduate degrees, in which the curriculum reproduces, at least in part, the GA model. This means that even though university-specific postgraduate qualifications provide specialized and accredited training in audiology, these degrees do not allow practicing as GA or HAS after graduation. As a result, the qualification and professional profile of the GA has never formally existed in Spain. The appearance of these degrees has caused that four professional profiles of HAS currently exist in Spain: Professionals with the vocational training certificate in HAS only, professionals with vocational training certificate and postgraduate qualifications in audiology, professionals with vocational training certificate and undergraduate degree in audiology-related discipline, and, finally, professionals with vocational training certificate, undergraduate degree in audiology-related discipline and postgraduate qualifications in audiology. The objective of this study was to compare the workplaces, the services offered and the self-perceived quality of their training of the different profiles of HAS currently existing in Spain, and to examine whether any of these professional profiles currently implement professional activities competence of the GA model. Our hypothesis was that HAS with a postgraduate qualifications in audiology and/or undergraduate degree in audiology-related discipline would show better self-perception of their training and more varied professional competencies than those with the HAS vocational training only. In addition, we hypothesized that HAS with a postgraduate qualifications in audiology and/or undergraduate degree in audiology-related discipline would perform their professional work more frequently in workplaces outside hearing aid or optical centers and that they would offer a wider range of services than HAS with only the vocational training certificate. Therefore, HAS with postgraduate qualifications in audiology and/or undergraduate degree in audiology-related discipline would show a professional profile closer to the GA than professionals with only a degree in HAS.
Methods
Questionnaire
A questionnaire was developed on the Google Forms platform (available in the Supplementary Material). HAS who developed their professional services in Spain were targeted for data collection. The questionnaire was disseminated online. Participants completed the questionnaire voluntarily and anonymously and received no compensation for their participation. The study was approved by the Vanderbilt University Institutional Review Board (USA).
The questionnaire was divided into three sections: Demographic questions (7), professional services questions (12) and audiology training questions (12). Demographic questions included the age of participants, gender, education and training received, the autonomous community where they practiced as HAS, and their current workplace/s. The workplaces were divided into hearing aid centers (independent and chain), optical centers3 (independent and chain), early intervention centers, schools (institutes, universities, or private centers), manufacturers, private hospital or ENT clinics, public hospitals and unemployed.
Professional performance questions focused on the populations attended (pediatric or adult) and the type of service offered (counselling and adaptation of hearing aids and cochlear implants, as well as evaluation and treatment of vestibular disorders). In addition, questions on the implementation of evidence-based clinical practices were included, specifically performing real-ear measurements (REM) when fitting hearing aids. This question is characteristic of the professional practice questionnaire since REM are used as an indicator of good practices because the use of this clinical protocol predicts patient satisfaction in the hearing-aid fitting process (Aarts & Caffee, 2005; Kirwood, 2010; Mueller & Picou, 2010). Professional performance responses were organized on a Likert scale of one to four (1 = never, 4 = always).
Training questions focused on professionals' self-perceptions on their overall training as well as on specific areas of audiology (hearing aid fitting and counselling, bone-anchored hearing-aids [BAHA], and cochlear implant programming and counselling). In addition, they were asked how they would perceive the creation of an official undergraduate degree in audiology in Spain, whether they thought that the quality of the audiology training in Spain was at the same level as in other countries and, if in general, they perceived they had good enough training to perform their daily clinical practice. The answers to the questions in the training section were organized on a Likert scale of one to four (1 = strongly disagree, 4 = strongly agree). Finally, it should be noted that in the present study we analyzed a sub-sample of the questions included in the questionnaire, which are relevant to answering our research questions. Results of questions not included in this study are available upon request.
Participants
Two hundred and ninety-two participants completed the questionnaire between May and December 2018. Of these, 33 indicated that they were not qualified as HAS, so their responses were discarded. Of the remaining sample, four other questionnaires were discarded because professionals reported currently working outside Spain (three in South America and one in the United Kingdom). As a result, 255 questionnaires were selected for this study. One hundred and seventy-six were completed by women and 79 by men. The most represented age group was 25-35 years with 102 participants, followed by 35-45 years with 90 participants, 45-55 years with 37 participants, 18-25 years with 17 participants and >55 years with 9 participants. The autonomous communities of origin are represented in Table 1. Moreover, from the 255 HAS in total, 186 (72%) did not report having any additional degree beyond the vocational training (HAS), 11 participants (4%) had obtained a postgraduate qualification in audiology (HAS+G) in addition to the vocational training4 . 41 (16%) had obtained a university degree in an audiology-related discipline (HAS+U) and 17 (7%) a postgraduate qualification in audiology and a university degree in an audiology-related discipline (HAS+UG).
Table 1: Distribution of participants by autonomous community
Autonomous community |
% |
Community of Madrid |
27 |
Valencian Community |
14 |
Andalusia |
13 |
Catalonia |
9 |
Castilla y León |
6 |
Basque Country |
6 |
Others |
25 |
The question about autonomous communities was included to the questionnaire after its release so only 159 participants are represented. Cantabria, Ceuta, and Melilla were not represented in the questionnaire. |
|
Analyzes
To analyze workplaces the total number of responses for each category from this question (each participant was able to mark more than one workplace), and the percentage of responses for each workplace category were computed over the total number of responses. To analyze whether there were differences between the groups (HAS, HAS+U, HAS+G, HAS+UG) on their most common workplaces, a chi-square test of heterogeneity with Monte-Carlo simulation was performed with workplace categories as a dependent variable, and group as an independent variable. In addition, post-hoc chi-square analysis was performed to analyze which groups differed from each other on the distribution of workplaces.
To analyze whether there were differences between the groups in terms of the services offered and the self-perceived quality of their training, one-way within-subjects analysis of variance (ANOVA) was conducted for each of the service and training questions. In all ANOVAs, the score provided for each question (between 1 and 4) served as the dependent variable, while group (HAS, HAS+U, HAS+G, HAS+UG) served as the independent between-subject variable. In all cases, when the results of the overall ANOVAs (omnibus) were significant, post-hoc analyzes were performed to analyze differences between the different groups. In cases of violation of sphericity assumptions, ANOVAs p-values were computed with Huynh-Feldt correction. Finally, in all post-hoc analysis, the false-discovery rate of Benjamini and Hochberg was used to correct for multiple comparisons.
Results
Workplaces
In general, considering the entire sample, we observed that hearing aid or optical centers (82%) were the workplaces in which participants indicated to develop most frequently their professional activity. Other workplaces indicated were private ENT clinics or hospitals (private and public; 6%), hearing-aid manufacturers (5%), teaching centers (3%), and early intervention centers (2%). Only 2% of the total sample indicated that they were unemployed (see Table 2). The groups from the sample (HAS, HAS+U, HAS+G, and HAS+UG) differed significantly on their workplaces (χ2 = 60,84 p < 0,01). Post-hoc analysis indicated that this difference was between the HAS+UG group and the HAS group (p < 0,01) and between the HAS+UG group and the HAS+U group (p < 0,01). For example, HAS+UGs worked more frequently in early intervention centers (10.5%) or hospitals (5%) than the rest of the groups (0%; Table 2).
Table 2: Percentage of responses per workplace type for each group
Total Sample (n = 255) |
Groups |
||||
HAS (n = 186) |
HAS+U (n = 41) |
HAS+G (n = 11) |
HAS+UG (n = 17) |
||
Optical Center (chain, 5 centers or more) |
14.0% |
15.0% |
15.5% |
15.5% |
0.0% |
Independent optical Center (5 centers or less) |
10.5% |
8.0% |
24.5% |
0.0% |
5.0% |
Hearing Aid Center (chain, 5 centers or more) |
31.0% |
35.5% |
24.5% |
15.5% |
10.5% |
Independent Hearing Aid Center (5 centers or less) |
27.0% |
24.0% |
22.5% |
46.0% |
53.0% |
Early Intervention Center |
2.0% |
1.0% |
2.0% |
0.0% |
10.5% |
Private ENT hospital or clinic |
5.0% |
5.5% |
2.0% |
7.5% |
5.0% |
Public hospital |
0.5% |
0.0% |
0.0% |
0.0% |
5.0% |
Teaching Center (Audiology) |
3.0% |
2.5% |
4.5% |
0.0% |
10.5% |
Manufacturer |
5.0% |
6.0% |
2.5% |
15.5% |
0.0% |
Unemployed |
2.0% |
2.5% |
2.0% |
0.0% |
0.0% |
HAS = Hearing-Aid Specialist; HAS+U = Hearing-Aid Specialist with an Undergraduate degree in audiology-related discipline; HAS+G = Hearing-Aid Specialist with a (post)Graduate qualification in audiology; HAS+UG = Hearing-Aid Specialist with an Undergraduate degree in audiology-related Discipline and a (post)Graduate qualification in Audiology. Percentages can add up to more than 100% because participants could indicate more than one workplace. |
|||||
Audiology services
In general, considering the entire sample, we observed that a large majority of the participants indicated conducting hearing aid counselling and fitting frequently (92%), followed by bone-anchored hearing aids counselling and fitting (23%), cochlear implants counselling and fitting (14.5%) and diagnosis and treatment of vestibular disorders (10%; See Figure 1). In addition, most of the participants indicated providing services to adult patients (93%), while the number of participants who indicated providing services to patients under 18 and under 5 years old was lower (34% and 20%, respectively; see Figure 2). 65% of the sample indicated conducting real-ear measurement during hearing-aid fitting (good practices). Finally, 22% of the sample indicated that their patients were frequently advised on the different communication methods (oral language, sign language, etc.). The ANOVAs performed to compare the types of service offered between the groups revealed significant differences in some of the questions. Specifically, the groups differed significantly on the frequency of cochlear implants counselling and programming (F3,251 = 3,5, p < 0,05, η2G = 0,04) and on provision of information related to communication options to their patients (F3,251 = 6,8, p < 0,001, η2G = 0,08). Post-hoc analysis revealed that HAS+UG provided significantly fewer services related to cochlear implant counselling and programming than HAS (p < 0,05) and HAS+U (p < 0,05). In addition, participants with HAS+UG provided more frequently information to their patients on communication options than HAS (p < 0,001) and HAS+U (p < 0,05). No differences were found between any of the groups in the remaining questions related to audiology services (hearing aids, bone-anchored hearing aids, or balance disorders; see Figure 1).
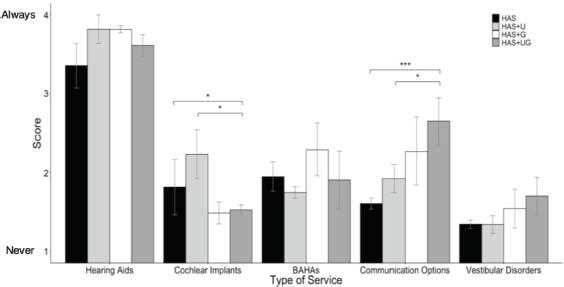
Figure 1. Average scores across participants regarding questions related to “type of service”. HAS = Hearing-aid Specialist; HAS+U = Hearing-aid Specialist with Undergraduate degree in audiology-related discipline; HAS+G = Hearing-aid Specialist with (post)Graduate qualifications in audiology; HAS+UG = Hearing-aid specialist with undergraduate degree in audiology-related discipline and postgraduate qualifications in audiology; BAHA = Bone-anchored hearing aid. * p < 0.05; *** p < 0.001.
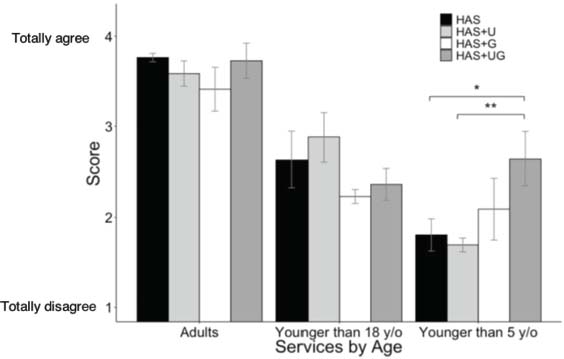
Figure 2. Average scores across participants regarding questions related to services provided by age. HAS = Hearing-aid specialist; HAS+U = Hearing-aid specialist with undergraduate degree in audiology-related discipline; HAS+G = Hearing-aid specialist with postgraduate qualifications in audiology; HAS+UG = Hearing-aid specialist with undergraduate degree in audiology-related discipline and postgraduate qualifications in audiology; y/o = years old. * p < 0.05; ** p < 0.001
The ANOVAs performed to compare the types of services offered by age between the groups revealed significant differences on the number of children under five years of age attended (F3,251 = 4,4, p < 0,01, η2G = 0,05). Post-hoc analysis revealed that HAS+UG attended more frequently children under five years of age than HAS (p=0.,01) and HAS+U (p=0,05). No differences between the groups on any other question related to services provided by age were found (adults and children under 18 years of age; see Figure 2).
Self-perceived quality of training
In general, considering the entire sample, we observed that a high percentage of participants (87%) indicated that they had sufficient training to implement their daily audiological practice. However, only 26% indicated that audiology training in Spain was at the same level as other surrounding countries. Regarding the education received, almost all participants (94.5%) indicated that they had adequate training to evaluate, counsel and fit patients with hearing aids. In contrast, 36% and 21% of participants reported having received adequate training to evaluate, counsel, fit, and program BAHA and cochlear implants, respectively. In addition, a high percentage of the sample reported having sufficient training to put scientific information into practice on their daily work (65%) and to seek continuous training opportunities (89%). In addition, most participants (90%) indicated that an undergraduate degree in audiology was necessary in Spain and that they would try to complete it, if possible (94.5%). Finally, 23% of participants noted that a degree in audiology would pose a threat to their current job.
ANOVAs performed to compare self-perceived quality of training among groups revealed significant differences in cochlear implant programming and counselling training (F3,251 = 4,5, p < 0,01, η2G = 0,05; see Figure 3). Post-hoc analysis revealed that HAS+UG provided significantly fewer services related to cochlear implant counselling and programming than HAS (p < 0,01) and HAS+U (p < 0,01). No differences were found between any of the groups in the rest of the training-related questions (hearing aids and bone-anchored hearing aids). Therefore, there were no significant differences between the groups implementing good clinical practices, seeking continuous training or on the need to create a degree in audiology in Spain, among others.
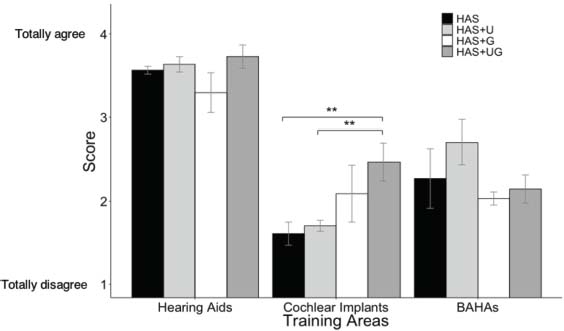
Figure 3. Survey average scores across participants regarding self-perceived training questions by audiology area. HAS = Hearing-aid specialist; HAS+U = Hearing-aid specialist with undergraduate degree in audiology-related discipline; HAS+G = Hearing-aid specialist with postgraduate qualifications in audiology; HAS+UG = Hearing-aid specialist with undergraduate degree in audiology-related discipline and postgraduate qualifications in audiology; BAHA = Bone-anchored hearing aid; ** p < 0.01
Discussion
The purpose of this study was to explore whether the different Hearing-Aid Specialist (HAS) professional profiles currently existing in Spain differed in the workplaces, services offered and the self-perceived educational training, and examine if any of these professional profiles performed clinical activities characteristic of the general audiologist (GA). We compared four groups of professionals: HAS with vocational training certificate (HAS) only, HAS with undergraduate degree in an audiology-related discipline (HAS+U), HAS with postgraduate qualifications (HAS+G) and HAS with undergraduate degree in an audiology-related discipline and postgraduate qualifications in audiology (HAS+UG). The results indicated that, regardless of their educational level, most HAS from Spain (1) have no university education in the form of an undergraduate degree in audiology-related discipline or postgraduate qualifications in audiology (71%), (2) perform their professional clinical activities in hearing aid and optical centers, (3) limit their professional activities to hearing-aid fitting in adults, for what they perceived they had received adequate trained, and (4) do not show a professional profile similar to the GA model, because according to the European Federation of Audiological Societies (EFAS, 2001), GA's competencies extend to the treatment of hearing loss with bone-anchored hearing aids and cochlear implants, as well as the diagnosis and treatment of tinnitus and vestibular disorders.
Differences between groups by educational level: Workplaces
Regardless of the education level, most HAS developed their professional activities in hearing aid or optical centers. The percentage of HAS working in other workplaces was less than 20%. However, and partially according to our hypothesis, we found that HAS+UG worked more often than HAS and HAS+U in independent hearing aid centers and public hospitals. The HAS and the HAS+U worked more often in hearing aid centers from commercial chains and optical centers than the other groups. This is of interest because, despite of focusing on hearing-aid fitting, independent hearing aid centers tend to serve more often patients with special needs (e.g., pediatric population) than optical and hearing aid centers from commercial chain, which serve mainly elderly population with hearing loss. Independent hearing aid centers and hospitals may actively seek to hire HAS with higher education to provide more specialized services to their patients. Although HAS+UG are present in hospitals, the percentage is low (5%). It would be of interest to investigate which professionals are providing services characteristic of the GA in hospitals, ENT clinics or early intervention centers. Future research studies could investigate the training and competencies of other hearing health professionals, as well as patient satisfaction with the services received from these professionals to assess the possibility of improving audiology education in Spain.
Differences between groups by educational level: Services offered and training
We only observed differences between the groups in two questions related to services and training. The first difference was observed in services provided to patients under five years old, who are treated more frequently by HAS+UG than by HAS and HAS+U. This may be related to the fact that HAS with higher education levels are more present in specialized hearing aid centers, early intervention centers, and public hospitals than those with lower education levels. The second difference was found in cochlear implant programming, where HAS+UG indicated that they felt more trained than HAS and HAS+U. However, HAS+UG offered services in this area less frequently than the other two groups. This could be explained by the fact that some large hearing aid centers from commercial chains, where there is a higher prevalence of HAS with no postgraduate qualifications in audiology, provide cochlear implant programming services. Therefore, some of these professionals (HAS and HAS+U) may have to counsel and programme cochlear implants even though they do not perceive themselves as sufficiently trained in this area. However, regardless of their education level, the frequency at which professionals offered implant programming services was low in all groups. Therefore, it is possible that other hearing health professionals (ENTs, implant manufacturer engineers, etc.) are conducting professional activities characteristic of the GA. Future studies should meticulously define which professional performs cochlear implant programming, the training received, and the quality of the service. In general, a large majority of HAS perceived themselves to be primarily trained for fitting hearing aids to adults and indicated offering this service more frequently than any other.
Finally, regardless of the educational level, the professionals indicated that the level of audiology training in Spain was not comparable to other countries and that they saw a need to create an undergraduate degree in audiology. These responses are likely motivated by the lack of training indicated by professionals in certain areas of audiology. However, most participants indicated that they were sufficiently trained to perform their daily clinical tasks, which focus on fitting hearing aids to adult patients. In addition, the percentage of participants who indicated implementing good practices by using REM is comparable to those reported in other countries such as the United Kingdom or the United States (~65%; Aarts & Caffee, 2005; Kirwood, 2010; Mueller & Picou, 2010).
Therefore, based on the survey´s data, the audiology training system in Spain is not ready to provide a professional profile that resembles the general audiologist model. Future studies could include professionals from audiology-related disciplines (engineers, ENTs, speech therapists, and other health personnel) to provide a comprehensive overview of the situation of audiology in Spain. National audiology associations need to conduct studies that include all professionals, their training, and the services they offer, as well as indices of patient satisfaction. Depending on the results obtained, the creation of an undergraduate degree in audiology in Spain that complements the current HAS vocational training could be considered and perhaps promoted. By doing this, GAs could be trained in Spain following the model proposed by EFAS. As a result, the professional profile of the GA could emerge and be recognized, opening areas of professional activities that nowadays seem to be inaccessible to HAS. This could potentially improve hearing health services.
Limitations
The results of this study were based on HAS self-perceived answers using a digital questionnaire. No direct observations were obtained on their professional performance. Although it is a very common practice to analyze professional performance with questionnaires (Aarts & Caffee, 2005; Kirwood, 2010; Mueller & Picou, 2010), it is important to remember that questionnaires have their limitations. The main limitation being the social acceptance bias that causes respondents answering in a socially acceptable manner. Some of the strategies that prevent social acceptance bias are to inform respondents that the results are anonymous, to use a questionnaire instead of an interview, or using multiple choice questions instead of open questions. All these strategies were included in the questionnaire used in this study. In addition, this study is limited by differences in sample size between the groups which could affect statistical power to detect significant differences between groups. Therefore, interpretation of the results must be taken with caution until future research studies replicate these findings.
Conclusion
Data from this study indicate that regardless of whether they have completed university training in the form of an undergraduate degree in an audiology-related discipline or graduate degree in audiology, most of the HAS in Spain develop their professional work adapting hearing aids to adult patients in hearing aid centers. HAS with a university degree in audiology and an undergraduate degree in an audiology-related discipline receive a more specialized training, which allows them to work more frequently in independent hearing aid centers and in some cases in early intervention centers and hospitals. However, this training does not allow them to conduct, on a general basis, the professional activities characteristic of the GA, such as cochlear implant programming, bone-anchored hearing aid fitting, treatment of balance disorders or pediatric care. Therefore, current HAS training (with or without a postgraduate qualifications in audiology) does not generate professionals capable of conducting the professional activities of the GA. The audiology situation in Spain needs a more detailed analysis to assess the quality of the services offered to patients with hearing difficulties, as well as possible modifications of educational training to comply with the recommendations of EFAS.
References
Aarts, N. L., & Caffee, C. S. (2005). Manufacturer predicted and measured REAR values in adult hearing aid fitting: Accuracy and clinical usefulness. International Journal of Audiology, 44(5), 293-301. https://doi.org/10.1080/14992020500057830
American-Speech-Language-Hearing Association (2020, May 8). Hearing and Balance. Retrieved from https://web.archive.org/web/20200508060253/https://www.asha.org/public/hearing/.
European Federation of Audiology Societies (EFAS). (2001) Audiology in Europe. Retrieved from https://web.archive.org/web/20191224091707/http://www.efas.ws/noticeboard/general_audiologist.htm. Accessed April 20, 2020.
Goulios, H. (2010). Comparative audiology and the development of a seeding model for affordable and sustainable audiology education (Doctoral Thesis, University of Western Australia, Australia). Retrieved from https://research-repository.uwa.edu.au/en/publications/comparative-audiology-and-the-development-of-a-seeding-model-for-
Goulios, H., & Patuzzi, R. B. (2008). Audiology education and practice from an international perspective. International Journal of Audiology, 47(10), 647-664. https://doi.org/10.1080/14992020802203322
Kirkwood, D. H. (2010). Survey probes dispensers' views on key issues raised by consumer reports. The Hearing Journal,63(5), 17-18. https://doi.org/10.1097/01.HJ.0000373446.75826.e1
Mueller, H. G., & Picou, E. M. (2010). Survey examines popularity of real-ear probe-microphone measures. The Hearing Journal, 63(5), 27-28. https://doi.org/10.1097/01.HJ.0000373447.52956.25
Order SCO/1262/2007, Approving and publishing the training programme for the specialty of Otorhinolaryngology (2007). Official State Gazette (BOE). núm. 110, de 8th May 2007, 19880-19889. https://www.boe.es/eli/es/o/2007/04/13/sco1262
Royal Decree-Law 1685/2007, Establishing the minimum competences of the vocational training in Hearing-Aid Specialist. (2008) Official State Gazette (BOE), núm. 13, 15th January 2008, 2615-2638. https://www.boe.es/eli/es/rd/2007/12/14/1685
Supplementary Material
https://journal.auditio.com/auditio/libraryFiles/downloadPublic/16
Conflict of interest
The authors declare that they have no conflict of interest. This research study was conducted in the absence of commercial or financial relations that could be interpreted as a potential conflict of interest.
Funding
This investigation has not received external funding.
Data Availability Statement
Data is not publicly available.
Acknowledgments
We thank Javier Santos for the conceptualization of the study, as well as his active participation in the development of the survey and data collection. In addition, we thank Anne Marie Tharpe for her willingness to act as a mentor in the study authorization process by the Vanderbilt University Institutional Review Board.
Contributions of the authors
Carlos Benitez Barrera and Beatriz de Diego-Lazaro have contributed equally to the conceptualization, data collection, drafting, revision, editing of the manuscript, data analysis, methodology and visualization.
_______________________________
1 The medical audiologist is a professional figure that, unlike other European and Latin American countries, does not exist in Spain. The medical audiologist receives a basic medical training and then specializes in audiology, without necessarily becoming an ORL.
2 Vocational training are certified professional studies alternative to college that provide theoretical and practical skills, offering hands-on training, and enabling fast incorporation to the labour market.
3 In Spain, optical centers with a certified hearing-aid specialist are authorized to dispense hearing aids. As a result, many HAS work in these type of healthcare facilities.
4 For some the university-specific degrees in audiology, Spanish universities admitted HAS without a university degree in their courses during the first years of implementation.
How to cite:
Benitez-Barrera, C. R., & De Diego-Lázaro, B. (2021). Educational Training and Services provided by the hearing-aid specialists : A comparison with the General Audiologist Model. Auditio, 5(3), e78.
https://doi.org/10.51445/sja.auditio.vol5.2021.0078
*Correspondence
Carlos R. Benitez-Barrera is now at Callier Center for Communication Disorders at the University of Texas at Dallas, 1966 Inwood Road, Dallas, TX, 75235
email: carlos.benitez-barrera@utdallas.edu
†Equal contribution
 CC-ND-BY 4.0
CC-ND-BY 4.0
© 2021 Los autores / The authors
Editorial Office
Copyeditor: Tomás Pérez Pazos.
Translation: Louis M. de Ladebauche
Trans. Revision: BenÍtez-Barrera y Sanchez-Lopez
Production: Publicaciones Académicas